Thoa sought care at Tam Anh General Hospital Ho Chi Minh City after two weeks of worsening fatigue, occasional chest discomfort, and mild shortness of breath. Dr. Pham Thuc Minh Thuy, a specialist in congenital cardiology at the Cardiovascular Center, reported the patient's heart rate was 49 beats per minute, significantly below the normal 60-90 bpm. An echocardiogram identified two atrial septal defects, measuring 12.7x6.1 mm and 11.5x4.4 mm, and a dilated right heart chamber.
Atrial septal defect (ASD) is a common congenital heart defect often diagnosed in adulthood, especially in women. Normally, a sealed septum separates the heart's two upper chambers. An ASD creates a hole in this septum, causing blood to flow from the left atrium to the right. This redirects oxygen-rich blood, meant for the body, back to the lungs, mixing with deoxygenated blood and leading to insufficient oxygen supply. This abnormal flow overworks the heart, which can eventually lead to dilated heart chambers, arrhythmias, heart failure, and pulmonary hypertension due to the increased blood volume in the lungs.
Dr. Vu Nang Phuc, Head of the Congenital Cardiology Department at the Cardiovascular Center, explained that ASD often shows no early symptoms. Many individuals remain unaware of their condition until screening or when complications cause noticeable heart dilation. In adults, an atrial septal defect larger than 7 mm causes blood shunting, leading to right heart overload and a higher risk of pulmonary hypertension over time. Thoa's heart had two large defects, necessitating intervention with an occluder device to preserve long-term heart function.
The patient's combined defect length measured 29 mm, with the two defects separated by a narrow 8 mm. The intervening tissue was thin and highly mobile. Closing each defect with separate devices carried a risk of displacement due to the mobile septum. Doctors opted for balloon dilation to break down the thin tissue between the two defects, merging them into one. This larger defect was then closed with a single 36 mm diameter occluder device. This larger device offers a wide gripping area, closely conforming to the heart's structure, reducing displacement risk compared to two smaller devices and simplifying intracardiac procedures.
The entire procedure was performed under X-ray guidance. Post-intervention checks confirmed complete closure by the device, with no impact on adjacent structures. Thoa was conscious, breathing well, and discharged after one day.
 |
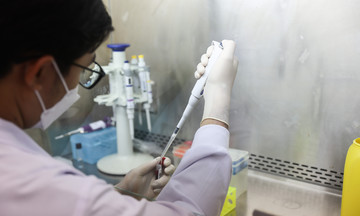
Dr. Phuc performs an atrial septal defect closure on a patient. Illustration: Huyen Vu |
Transcatheter atrial septal defect closure is a minimally invasive procedure offering several advantages: it is safe, involves minimal blood loss and pain, reduces infection risk, and ensures rapid recovery without open-chest surgery or scarring. Patients can resume normal activities immediately after the intervention.
Dr. Thuy stated that atrial septal defects cannot be prevented. Individuals diagnosed with the condition should maintain a healthy lifestyle. Patients should exercise regularly, follow a diverse, nutrient-rich diet including vegetables and grains, and limit bad cholesterol. Avoiding infections is crucial, as congenital heart disease increases the risk of pneumonia and respiratory infections.
Women with atrial septal defects and severe pulmonary hypertension should consult a doctor if they plan to become pregnant. Family members of ASD patients should undergo examinations and echocardiograms to rule out their own risk.
Thu Ha
* Patient's name has been changed
| Readers can submit questions about cardiovascular disease here for doctors to answer. |