At Tam Anh District 7 Polyclinic, non-invasive prenatal testing (NIPT) at 10 weeks of gestation, combined with genetic screening, indicated a low risk for chromosomal abnormalities in the pregnant woman. The 28-year-old mother had a heterozygous SEA deletion linked to Alpha Thalassemia. Dr. Nguyen Hoang Long, a fetal medicine specialist, stated this heterozygous mutation does not cause disease in the mother but can be inherited by the child. Her husband's gene test confirmed he did not carry a similar abnormal gene, eliminating the need for further fetal genetic testing.
At 36 weeks of gestation, an ultrasound recorded the fetal weight at the 16th percentile, with normal placenta, amniotic fluid, and PSV-MCA index (assessing fetal anemia). The fetus had a pericardial effusion of 4,3 mm, with localized thickening of the left ventricle: lateral wall 5,9 mm, posterior wall 5,7 mm, and interventricular septum 4,4 mm.
Fetal pericardial effusion is the accumulation of fluid measuring 4 mm or more within the pericardium. Normally, a thin layer of fluid in the pericardial cavity reduces friction between the heart and surrounding structures. When this fluid layer thickens, it puts pressure on the heart, affecting its pumping function. Causes of fetal pericardial effusion can include chromosomal abnormalities or genetic conditions such as Down, Edwards, Turner, or Noonan syndromes.
Other risk factors include fetal heart defects or other congenital malformations, maternal viral infections such as Parvovirus B19 and Cytomegalovirus (CMV), fetal anemia, or maternal autoimmune disorders. In some cases, the cause remains unknown.
According to Dr. Long, the ultrasound results and the fetus's health condition strongly suggested isolated pericardial effusion. Subsequent ultrasounds showed no further progression of the pericardial effusion, fetal heart function remained normal, and no other accompanying abnormalities were observed on ultrasound. The pregnant woman continued to monitor her pregnancy according to the routine prenatal check-up schedule.
At 40 weeks of gestation, a baby girl was born, weighing 2,8 kg. The baby's echocardiogram 24 hours after birth showed no progression of the pericardial effusion. Three days later, the condition decreased, and both mother and baby were stable and discharged from the hospital.
 |
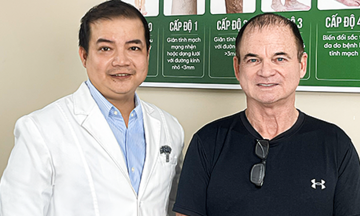
Obstetrics and Gynecology team performing a C-section for the pregnant woman. *Photo: Thuy Nguyen* |
Pericardial effusion can vary in severity; from a small amount of fluid to a large effusion, it can affect heart function. In some cases, it may be part of the progression of hydrops fetalis, a serious condition characterized by widespread fluid accumulation in the fetal body.
Dr. Long stated that morphology ultrasound and specialized fetal echocardiography help diagnose pericardial effusion, detect structural defects, and assess fetal health. Genetic and chromosomal tests, along with maternal infection screenings, help identify the cause. Depending on the case, doctors advise on monitoring, treatment, and screening for the infant immediately after birth.
Doctors recommend pregnant women with fetal abnormalities seek care at specialized medical centers with multidisciplinary collaboration to ensure a comprehensive assessment of the health of both mother and baby.
Ngoc Chau
| Readers can ask questions about obstetrics and gynecology here for doctors to answer |