A 31-year-old mother, married for 10 years, faced infertility due to blocked fallopian tubes. Despite undergoing tubal surgery, she couldn't conceive naturally, and three in-vitro fertilization attempts were unsuccessful.
In 2024, the couple had a successful embryo transfer. The mother received preeclampsia prophylaxis with aspirin at 12 weeks and cervical cerclage at 14 weeks due to a shortened cervix. The first trimester was challenging, with severe morning sickness, stress, and a high-risk pregnancy.
During a gestational diabetes test at 25 weeks at Tam Anh General Hospital in Ho Chi Minh City, she was diagnosed with severe preeclampsia with blood pressure exceeding 180/100 mmHg and abnormally high proteinuria. She had experienced swollen feet and headaches for about two weeks but dismissed them as normal pregnancy symptoms, delaying medical attention.
The obstetrics and gynecology team worked to prolong the pregnancy until 26 weeks. However, with her blood pressure remaining high, rapid heart rate, and fetal distress, an emergency C-section was performed. The baby girl was born weighing 750g with weak breathing. The neonatal team immediately implemented the "golden hour protocol," providing positive pressure ventilation and stabilizing her body temperature in the operating room. She was then transferred to the Neonatal Intensive Care Unit (NICU) and placed in an incubator.
Doctor Nguyen Minh Thanh Giang from the Neonatal Center explained that the extremely premature baby had severe respiratory distress, requiring surfactant administration to support lung function. Subsequently, she experienced prolonged apnea and cyanosis, necessitating intubation to maintain a clear airway. After 24 hours, her breathing improved, and she transitioned to non-invasive ventilation.
The baby's hemodynamic status was unstable due to an underdeveloped heart struggling to pump blood and oxygen throughout her body. The team closely monitored her blood pressure, administered vasoactive medications, and corrected acid-base imbalances to improve cardiac output. Doctor Giang noted that strict antibiotic management in the NICU allowed the baby to discontinue antibiotics early, avoiding the need for broad-spectrum antibiotics often required in extremely premature infants.
The baby received intravenous nutrition combined with early milk feeding, gradually increasing the milk volume. 20 days after birth, she transitioned to full oral feeding. However, a few days later, a brain ultrasound revealed a grade 2 brain hemorrhage. This occurred due to fragile blood vessels in the germinal matrix, damaged by factors related to extreme prematurity. A grade 2 hemorrhage signifies bleeding into the ventricles without ventricular dilation, but it carries the risk of progression to a more severe level with potential neurological complications. The team closely monitored her vital signs, controlled risk factors to prevent cyanosis and infections, and prevented further deterioration, as the blood vessels are highly sensitive to stress.
The team administered blood transfusions and erythropoietin to improve the baby's blood reserves. Born at 26 weeks, she missed the crucial blood storage phase that occurs during the last trimester (from 28 weeks), leading to anemia. The erythropoietin treatment lasted 4 weeks until her red blood cell count stabilized. Regular brain ultrasounds showed the blood clot resolving spontaneously after about a month. She was also weaned off the ventilator and began breathing with supplemental oxygen through nasal cannula.
 |
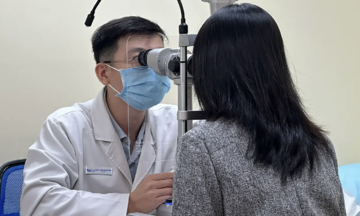
Doctor Giang examines the baby and guides the mother on how to care for her at home. Photo: Ngoc Chau |
Doctor Giang examines the baby and guides the mother on how to care for her at home. Photo: Ngoc Chau
Doctor Cam Ngoc Phuong, Director of the Neonatal Center at Tam Anh General Hospital, explained that the team implemented a family-integrated neonatal care model to encourage and facilitate parental involvement in the treatment process, contributing to the baby's recovery and development.
The mother's stress levels and ability to care for a premature infant were assessed. Based on this, the doctors developed a plan for training and psychological support for the mother alongside the baby's treatment. During her daily visits to the NICU, the mother received encouragement and support to build confidence for early skin-to-skin contact with her baby.
More than three months after birth, the baby's weight increased to 2.7 kg, equivalent to a 39-week gestation. She was breathing and feeding independently, and the brain hemorrhage was fully resolved. She received all necessary vaccinations and was discharged with scheduled follow-up appointments.
Ngoc Chau
| Readers can submit questions about children's health here for doctors to answer. |