After the miscarriage, Tinh took medication as prescribed to expel the fetal tissue, but experienced prolonged vaginal bleeding. At a local medical facility, doctors diagnosed an abnormal mixed mass in her uterus, measuring 9x6 mm. She was prescribed contraceptives to regulate her hormones, but the bleeding persisted.
She then sought treatment at Tam Anh General Hospital in Ho Chi Minh City. An ultrasound revealed multiple honeycomb-shaped echoes in her uterus, a characteristic sign of a molar pregnancy. Blood tests showed her Beta-hCG levels at 155,000 mIU/mL (significantly higher than in a normal pregnancy). An MRI confirmed a 4x5x6 cm mass within her uterus.
Dr. La Hong Chau, Head of the Obstetrics and Gynecology Imaging Unit at Tam Anh General Hospital in Ho Chi Minh City, explained that Tinh had developed gestational trophoblastic neoplasia (GTN), arising from the abnormal growth of placental tissue. In such cases, placental villi remaining after childbirth, abortion, or miscarriage degenerate and swell, forming fluid-filled sacs resembling a bunch of grapes or a honeycomb.
Gestational trophoblastic neoplasia encompasses a range of premalignant conditions like complete and partial molar pregnancies, as well as malignant forms such as invasive mole, choriocarcinoma, and placental-site trophoblastic tumor. In some cases, the placental tissue invades the uterine muscle, causing uterine perforation, spreading to surrounding organs and the abdominal cavity, or even metastasizing to distant organs like the lungs, liver, or brain.
According to Dr. Chau, diagnosing GTN requires considering the patient's pregnancy history. GTN typically appears after a pregnancy, including molar pregnancies, miscarriages, ectopic pregnancies, or even after a normal delivery. A molar pregnancy is considered the primary risk factor for GTN. The disease often manifests within the first 4 months following a dilation and curettage (D&C), miscarriage, or molar pregnancy treatment. Typical symptoms include prolonged vaginal bleeding, an enlarged uterus, and abnormally high Beta-hCG levels. Globally, the incidence of molar pregnancy ranges from 1/500 to 1/1,000 pregnancies. The frequency is higher in Asia, the Middle East, and Africa, and lower in Europe and the US.
 |
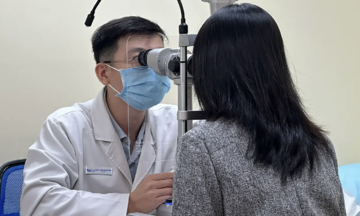
Ultrasound monitoring after a miscarriage. Illustrative photo: Tam Anh General Hospital |
Ultrasound monitoring after a miscarriage. Illustrative photo: Tam Anh General Hospital
Dr. Chau emphasized that ultrasound and hCG testing enable early diagnosis, monitoring of progression, and post-treatment surveillance of GTN. Treatment decisions are based on a risk assessment score. Low-risk GTN is treated with single-agent chemotherapy, with a cure rate near 100%. High-risk GTN requires multi-agent chemotherapy and may involve hysterectomy or removal of metastases, with a cure rate of around 90%. Hysterectomy is considered for patients without metastasis who do not wish to have more children.
While the prognosis is generally positive, patients face procedures like D&C, regular Beta-hCG monitoring, potential chemotherapy, and delayed future pregnancies. The prolonged monitoring and treatment process can lead to anxiety, depression, and stress.
Tinh's case highlights how a miscarriage or early pregnancy loss with abnormal placental tissue can pose a risk of GTN if not closely monitored.
Doctors recommend that women who have experienced a miscarriage, D&C, or molar pregnancy adhere to follow-up appointments and undergo regular Beta-hCG monitoring until the results are negative. Women should seek immediate medical attention if they experience prolonged vaginal bleeding, an abnormally enlarged uterus, or a positive pregnancy test after a pregnancy loss.
Tue Diem
*The patient's name has been changed.
| Readers can submit questions about obstetrics and gynecology here for doctors to answer. |