A 35-year-old office worker from Quang Ninh, Vietnam, became self-conscious about gaining almost 70 kg after her second child. Instead of consulting a nutritionist, she opted for a "quick fix" by purchasing various weight loss pills from a pharmacy and online. The seller offered a "combo" that included diuretics, laxatives, fat-burning pills, and appetite suppressants, totaling 6 to 7 different medications.
Initially, she was thrilled with a rapid weight loss of 1 to 2 kg per week, believing she had found a miracle solution. However, after a few months, she began experiencing insomnia, rapid heartbeat, dizziness, and fatigue. Upon hospitalization, doctors diagnosed her with severe electrolyte imbalance, liver failure, and cardiac arrhythmia, all consequences of her polypharmacy. Doctor Nguyen Huy Hoang from the Vietnam Society of Underwater and Hyperbaric Medicine shared the case on 22/9, warning that continued self-medication could have been fatal. Doctor Doan Du Manh from the Vietnam Vascular Society cautioned that such rapid weight loss methods primarily cause dehydration and metabolic disorders, potentially leading to acute kidney failure and metabolic acidosis.
Another case involves Nam, a 25-year-old sales representative and amateur bodybuilder, who experienced a similar ordeal. Aiming to gain muscle mass, Nam consumed a high-protein diet and various supplements and muscle-building drugs heavily advertised online. During a health check-up at Hanoi Medical University Hospital, he was diagnosed with chronic kidney failure due to chronic interstitial nephritis. Doctors attributed his condition to the indiscriminate use of multiple supplements.
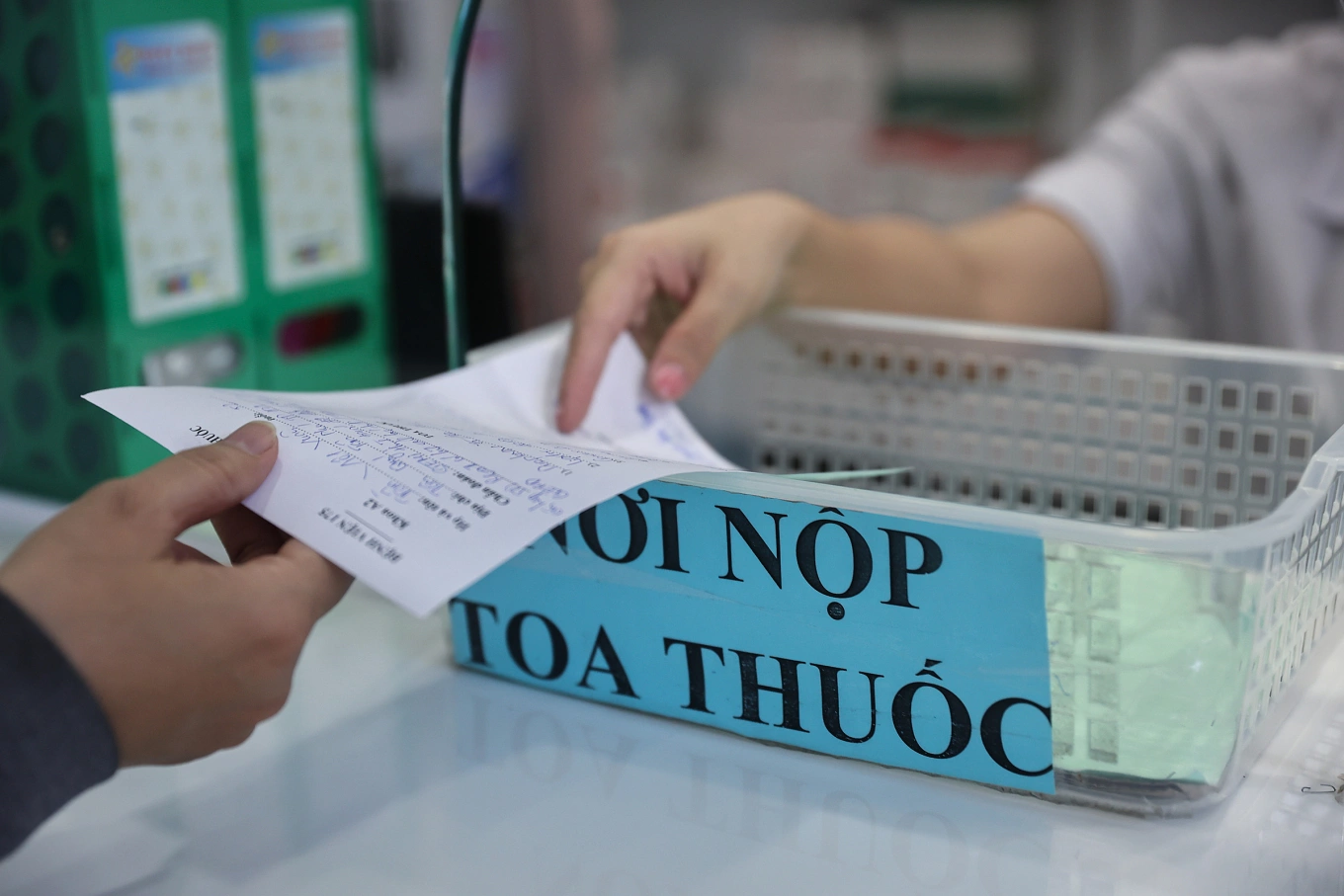 |
Pharmacy staff dispensing medication to a patient. Photo: Quynh Tran |
Pharmacy staff dispensing medication to a patient. Photo: Quynh Tran
This phenomenon is known as polypharmacy, the simultaneous use of 5 or more medications, including prescription drugs, over-the-counter medications, herbal remedies, and supplements. According to Dr. Hoang, this is a growing public health concern in Vietnam, though official statistics from authorities are lacking.
Combining multiple medications without medical supervision can lead to dangerous interactions. For example, mixing sedatives and antihistamines can cause excessive drowsiness; iron and calcium can reduce antibiotic absorption; and non-steroidal anti-inflammatory drugs (NSAIDs) can worsen hypertension and kidney problems.
Another risk is paracetamol overdose, a common ingredient in cold and pain relievers. Simultaneous use can lead to acute liver failure and even death. The liver and kidneys are particularly vulnerable when processing multiple active ingredients. Combining aminoglycoside antibiotics with NSAIDs increases the risk of kidney damage, while some products marketed as "liver protectors" can be toxic.
At the Vietnam Hospital Pharmacists Association Congress in August, Associate Professor Le Van Truyen, former Deputy Minister of Health, acknowledged the ongoing overuse of antibiotics. Patients taking unnecessary or inappropriate antibiotics contributes significantly to antibiotic resistance. A study published in the British Medical Journal (BMJ) found that unsupervised polypharmacy increases the risk of hospitalization in young people by 52%. The World Health Organization (WHO) warns that the misuse of medication contributes to the global antibiotic resistance crisis, projected to cause 10 million deaths annually by 2050.
To prevent this, Dr. Hoang recommends a multi-pronged approach involving individuals, regulatory bodies, and healthcare professionals. Patients should follow the WHO's "Know - Check - Ask" principle: thoroughly research information, verify product origins, and consult doctors or pharmacists before using any medication. They should also avoid reusing antibiotics or sharing them with others.
Regulatory bodies need to strengthen control over the sale of prescription drugs without prescriptions and implement a nationwide electronic prescription system. Doctors and pharmacists must uphold their responsibilities, prescribe evidence-based medication, refuse to sell drugs without prescriptions, and clearly warn about the risks of polypharmacy.
"This is not just a medical issue but also an ethical and systemic challenge, requiring action from everyone involved, from patients to policymakers," Dr. Hoang said.
Thuy Quynh