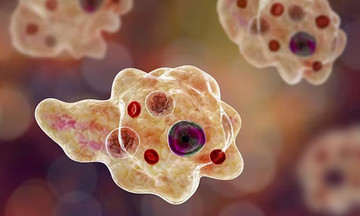
When Hoa visited Tam Anh General Hospital in Hanoi, she was 1.66 m tall, weighed 87 kg, and had a BMI of 31.3, indicating severe obesity. Her visceral fat measured 213 cm2 (the safe threshold is below 100 cm2), and over 50% of her body weight (44 kg) was fat. She also suffered from lipid disorders, prediabetes, and fatty liver disease.
Dr. Le Ba Ngoc, Head of the General Internal Medicine Department, created a weight loss treatment plan for Hoa, focusing on dietary changes and a scientific exercise regimen. Due to her severe obesity and several dangerous complications, she was prescribed injectable weight-loss medication to slow down gastric emptying and reduce appetite.
Nutritionist Dr. Tran Quyen An explained that extreme methods like prolonged fasting or completely cutting out carbohydrates can lead to rapid weight loss, but this is mainly due to loss of muscle and water, not visceral fat. This approach can also increase the risk of metabolic disorders. Hoa's goal was not rapid weight loss, but to reduce belly fat and visceral fat to improve her metabolic health sustainably. A proper calorie deficit diet provides enough protein and micronutrients, preserving muscle mass and enhancing visceral fat burning.
 |
Dr. An consults with a patient about their diet. Photo: Tam Anh General Hospital |
Dr. An consults with a patient about their diet. Photo: Tam Anh General Hospital
During the first month, Hoa reduced her daily calorie intake by 300-500 kcal compared to her maintenance needs. This moderate reduction helped avoid fatigue. Her daily menu included three main meals with a balanced energy distribution: 45-50% from complex carbohydrates (rice, oats, sweet potatoes, grains), 25-30% from lean protein (chicken, fish, lean meat, eggs, tofu), and 20-25% from healthy fats. Throughout the treatment, Hoa was guided to eat a variety of foods. Her protein intake was maintained at approximately 1.5-1.6 g/kg of ideal body weight per day to preserve muscle mass.
Hoa underwent regular Inbody assessments to track her visceral fat, skeletal muscle mass, water, minerals, protein, and basal metabolic rate. This tool not only provided initial diagnostic information but also monitored changes in her body composition throughout the treatment. Doctors used the Inbody results to accurately assess whether she was losing fat or muscle, adjusting her diet and exercise plan accordingly each week.
Her exercise routine focused on burning calories to create a calorie deficit, reduce visceral fat, increase muscle mass, and improve cardiovascular and respiratory health. Initially, she engaged in moderate-intensity aerobic exercises like brisk walking and cycling, gradually increasing the intensity to build muscle and boost energy expenditure.
According to Dr. Ngoc, Hoa's weight loss progress was closely monitored using regular Inbody assessments to evaluate various body composition indicators (visceral fat, skeletal muscle mass, water, minerals, protein, etc.) and basal metabolic rate. This provided both initial diagnostic information and ongoing tracking of her body's changes throughout the treatment. The Inbody results allowed doctors to precisely determine whether she was losing fat or muscle, enabling adjustments to her nutrition and exercise plan as needed.
After seven months of adhering to the multidisciplinary treatment plan, Hoa lost 25 kg. Her visceral fat area decreased to 92 cm2, and she avoided losing water or muscle. Her metabolic rate improved, and her blood sugar and lipid levels returned to normal. She continues to follow the recommended diet and exercise regimen to maintain a stable weight, prevent weight regain, and avoid accumulating visceral fat.
Mai Anh
*The patient's name has been changed.
| Readers can submit questions about endocrine diseases here for doctors to answer. |