Van, a 13-year-old girl with a history of being underweight and having a poor appetite, was found to have mild malnutrition with a body mass index (BMI) below 18. A transthoracic echocardiogram at Tam Anh General Hospital in Ho Chi Minh City revealed a 9 mm atrial septal defect (ASD) and an enlarged right heart chamber. A transesophageal echocardiogram confirmed the ASD, measuring it at 16 mm (medium-sized).
An ASD is a congenital heart defect characterized by a hole between the heart's two upper chambers (atria). Small holes often close spontaneously within a few weeks or months after birth. Doctor Pham Thuc Minh Thuy from the Congenital Heart Disease Department of the Cardiovascular Center explained that many children with ASDs are asymptomatic and develop normally, often leading to diagnoses during routine health checkups. Larger ASDs can cause symptoms like chest heaviness, sharp chest pain, shortness of breath, rapid breathing, fatigue, and recurrent pneumonia.
In Van's case, the ASD didn't close naturally but instead enlarged, leading to the right heart chamber's enlargement. The ASD increased blood flow to the right side of the heart and lungs, forcing them to work harder. Over time, this can cause complications such as heart chamber dilation, arrhythmia, heart failure, and pulmonary hypertension.
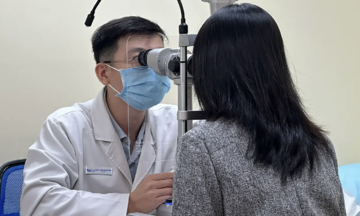
 |
Doctor Phuc examines Van's heart a week after the procedure. Photo: Ha Vu |
Doctor Phuc examines Van's heart a week after the procedure. Photo: Ha Vu
According to Doctor Vu Nang Phuc, Head of the Congenital Heart Disease Department at Tam Anh General Hospital in Ho Chi Minh City, medium to large ASDs require closure to prevent complications. The two common treatment options are catheter-based closure using a device and open-heart surgery to patch the hole.
Catheter-based closure is suitable for moderately sized ASDs (under 38-40 mm) with sufficient tissue rims (≥ 5 mm) to anchor the device. Van met the criteria for this less invasive procedure.
Van received local anesthesia in the groin area and remained conscious throughout the procedure. Before concluding, doctors performed a transthoracic echocardiogram to ensure the device was correctly positioned, without impinging on surrounding structures or causing heart valve leakage.
Van recovered swiftly and was discharged the next day. Doctors prescribed medication to prevent infective endocarditis and blood clots for six months. At her first follow-up appointment, Van was in stable condition, and the ASD closure device was functioning well.
Doctor Phuc noted that some ASDs can close spontaneously, so intervention isn't recommended for children under 1 year old without heart failure or significant pulmonary hypertension. Ideally, the procedure should be performed when the child is older, around 3-4 years of age. Delaying treatment can lead to structural and functional heart damage due to the enlarged ASD. Adults diagnosed with ASDs should consider closure before pulmonary artery pressure and resistance become too high.
Thu Ha
* The patient's name has been changed