Answer:
Pleural tuberculosis and pulmonary tuberculosis are both caused by infection with the tuberculosis bacterium (Mycobacterium tuberculosis), but they affect different parts of the body. Pulmonary tuberculosis occurs when the bacteria directly attack the lung tissue. Pleural tuberculosis is a condition where the bacteria cause inflammation in the lining surrounding the lungs, including the parietal and visceral pleura, leading to pleural effusion and potential adhesion of the two pleural layers.
About 80% of tuberculosis cases occur in the lungs, with pleural tuberculosis accounting for only 5-10%. However, many cases of pleural tuberculosis are a consequence of pulmonary tuberculosis, occurring when bacteria from the damaged lung tissue spread into the pleural cavity, causing inflammation and fluid buildup. The two diseases can occur simultaneously or sequentially, especially in people with weakened immune systems, with similar symptoms like coughing, fever, fatigue, chest pain, and shortness of breath.
To accurately diagnose pleural tuberculosis, doctors perform a clinical examination, chest X-ray, ultrasound, chest CT scan, pleural fluid aspiration for testing, blind pleural biopsy, or thoracoscopic pleural biopsy to look for tuberculosis granulomas. To diagnose pulmonary tuberculosis, doctors test sputum for AFB (smear microscopy and culture), Xpert MTB/RIF, MGIT in sputum, bronchoscopy, bronchial lavage, alveolar lavage, and biopsy.
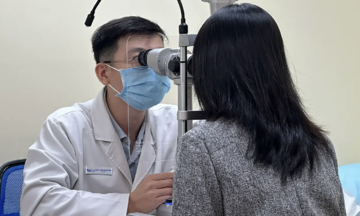
 |
Doctors perform pleural fluid aspiration for testing. Photo: *Tam Anh General Hospital* |
If you have pleural tuberculosis, you should also be screened for pulmonary tuberculosis to avoid missing an active or latent pulmonary focus, which can reduce treatment effectiveness and increase the risk of spreading the disease. Pleural tuberculosis alone, a form of extrapulmonary tuberculosis, does not pose a risk of transmission to others through the respiratory route. People with pulmonary tuberculosis can spread the bacteria when they cough, sneeze, or talk, creating a risk of infection.
Treatment for both diseases requires anti-tuberculosis medication following a regimen lasting over 6 months, depending on the condition. Both diseases impair respiratory function and carry the risk of recurrence or spread to other organs, but they have different complications.
With pulmonary tuberculosis, common complications include pneumothorax, bronchiectasis, and lung scarring. In pleural tuberculosis, common complications include pleural thickening, calcification, and pleural effusion, requiring pleural fluid drainage and breathing exercises to prevent pleural thickening. If you are diagnosed with pleural tuberculosis, you must adhere to the treatment and follow-up appointments for close monitoring and early detection of any related issues.
Preventive measures for both pleural and pulmonary tuberculosis include BCG vaccination for infants, maintaining personal hygiene and a well-ventilated living environment, and a healthy lifestyle. This includes a nutritious diet, regular exercise, and stress management. Limiting contact with people who have pulmonary tuberculosis and using appropriate protective measures are also important.
MSc. MD Phung Thi Thom
Department of Respiratory Medicine
*Tam Anh General Hospital* Hanoi
| Readers can submit respiratory disease questions here for doctors to answer. |