This deadline, effective 1/7, is part of the Ministry of Health's new circular regarding prescription regulations for outpatient treatment. Other healthcare facilities have until 1/1/2026 to comply.
This is the third time the Ministry has extended the deadline. Most recently, the deadline for healthcare facilities under circular 04/2022 to integrate their prescription systems was June 30, 2023.
Electronic prescriptions are a small but essential component of electronic health records. They are also used for outpatients who don't have health records. Nationwide use of electronic prescriptions is crucial for effective monitoring of prescription and dispensing practices.
The Ministry of Health has launched a national electronic prescription system to enhance transparency. The system integrates data such as facility codes, doctor codes, and prescription codes. It's expected to handle up to 600 million prescriptions annually.
On 6/7, Nguyen Huu Trong, General Secretary of the Vietnam Medical Informatics Association, stated that the national system aims to connect all prescriptions from public and private healthcare facilities nationwide. Each doctor, facility, and prescription will have unique identifiers linked to the Ministry of Health's central database.
With patient consent, the system will share prescriptions with pharmacies' software for dispensing. The system then receives reports on dispensed quantities for each prescription. This process prevents issues like using unverified handwritten prescriptions, refilling expired prescriptions, or exceeding prescribed quantities.
Paper prescriptions posed challenges in managing transparency and dispensing. Whether handwritten or computer-generated, they lacked verification of authenticity, prescriber authority, and dispensing status. This could lead to multiple refills, incorrect dispensing due to illegible handwriting, and potential health risks.
Despite legal frameworks, the adoption of electronic prescriptions has been slow. Factors include inadequate training, insufficient monitoring by authorities, and a lack of penalties, despite regulations being in place. "The rollout of electronic prescriptions has been delayed," Trong said.
Currently, only about 12,000 out of over 60,000 healthcare facilities regularly use the system. Many major hospitals haven't integrated their systems or only do so for insured patients, not those paying out-of-pocket. Most private clinics (around 40,000) also haven't connected. Out of over 218 million integrated prescriptions, only over 3.6 million outpatient prescriptions have been reported as dispensed.
Many facilities still use paper prescriptions, some even of dubious origin. Others use non-standard software or fail to integrate with the national system.
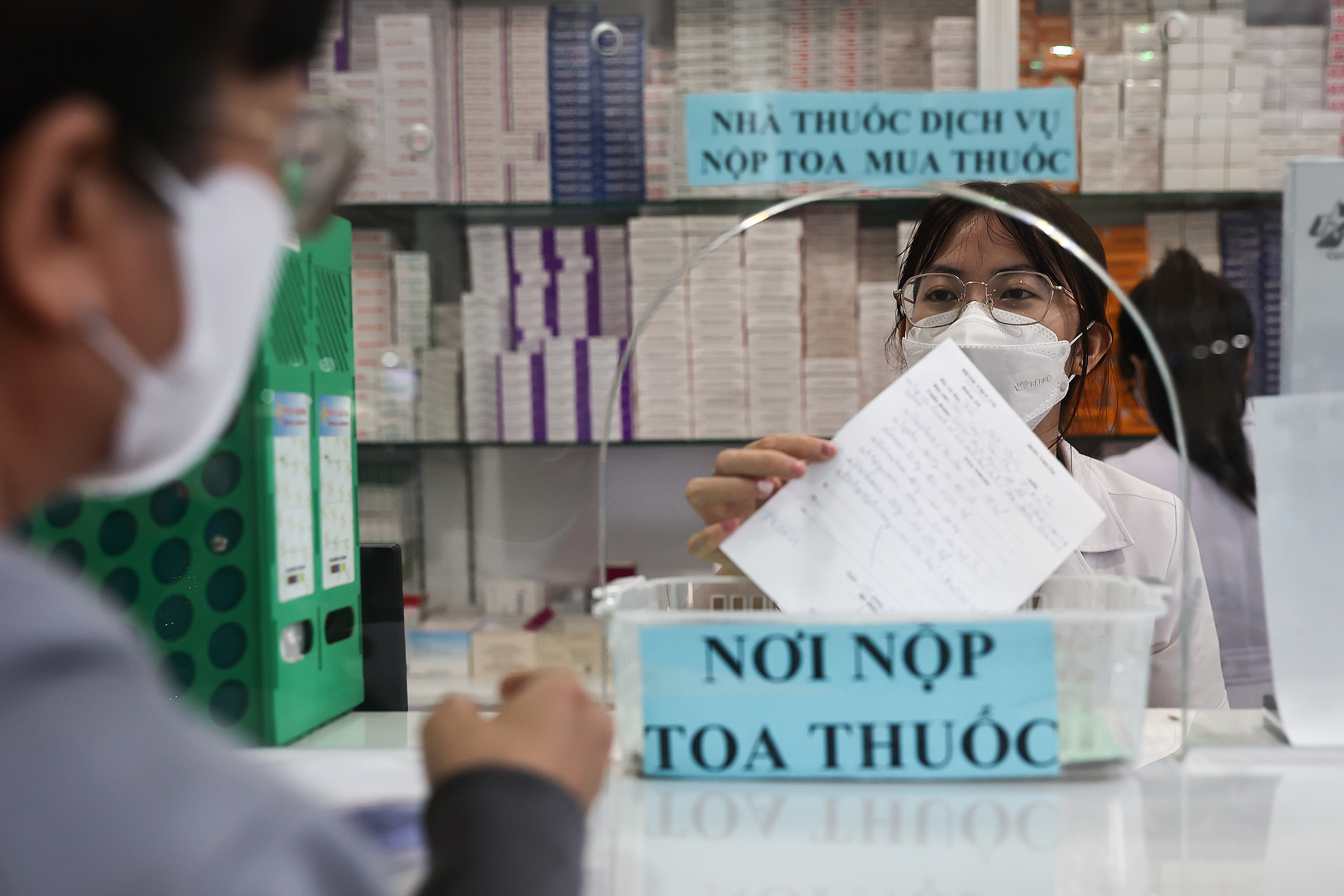 |
Medical staff at the pharmacy of 175 Military Hospital dispense medication to a patient. Photo: Quynh Tran |
Medical staff at the pharmacy of 175 Military Hospital dispense medication to a patient. Photo: Quynh Tran
According to Trong, integrating electronic prescriptions isn't technically difficult. It doesn't add extra steps to the doctors' workflow and streamlines dispensing for pharmacies. However, apprehension about increased transparency and regulatory scrutiny, along with a lack of financial incentives and enforcement, hinders adoption, especially among larger hospitals and private clinics. Some fear that increased transparency will expose malpractice such as unauthorized drug sales or improper prescribing.
Trong emphasizes the need for stricter monitoring of electronic dispensing and public awareness campaigns about using valid prescriptions. He urges the government to implement or strengthen penalties to ensure compliance from both healthcare facilities and pharmacies.
Le Nga












