Doctor Tran Luong Anh, Head of Neurosurgery and Spine at FV Hospital, explained on 29/7 that such tumors grow slowly and adapt to the skull, making them difficult to detect. Although the patient experienced occasional headaches, the tumor hadn't yet affected higher-level neurological functions. However, prompt surgery was crucial as further growth could lead to dangerous complications like seizures or become life-threatening.
Doctors consulted and determined that surgical removal posed a risk of damaging surrounding brain tissue due to the tumor's size and firmness. The tumor's extensive blood supply also presented a challenge, increasing the risk of significant blood loss during surgery.
 |
Doctors perform embolization on the patient before surgery. Photo: Hospital provided |
Doctors perform embolization on the patient before surgery. Photo: Hospital provided
To minimize blood loss and preserve blood vessels, Doctor Anh consulted with Doctor Huynh Huu Danh, an Interventional Radiologist from the Diagnostic Imaging Department. Doctor Danh performed an embolization procedure the day before the surgery to block the tumor's blood supply. This minimally invasive technique is used to treat various brain conditions, including cerebral arteriovenous malformations, cerebral aneurysms, carotid cavernous fistulas, and dural arteriovenous fistulas.
The embolization successfully blocked 90% of the tumor's blood supply. The following day, Doctor Anh's team performed the tumor resection guided by a neuronavigation system. This technology precisely defined the tumor's boundaries, optimized the surgical approach, and protected nearby blood vessels. The surgery also utilized an ultrasonic aspirator to address the tumor's firmness, preventing damage to surrounding brain tissue that might occur with manual removal.
The 4-hour surgery was successful, with the entire tumor removed. Blood loss was just over 200 ml, compared to the estimated 700-1,000 ml expected without prior embolization. Reduced blood loss facilitated the procedure, shortened the surgery time, minimized trauma to surrounding brain tissue, and eliminated the need for a blood transfusion.
"Blood transfusions always carry potential risks such as transfusion reactions or the transmission of bloodborne diseases," Doctor Anh explained. Significant blood loss can also disrupt the patient's blood clotting system, necessitating transfusions of clotting factors, which are both costly and risky.
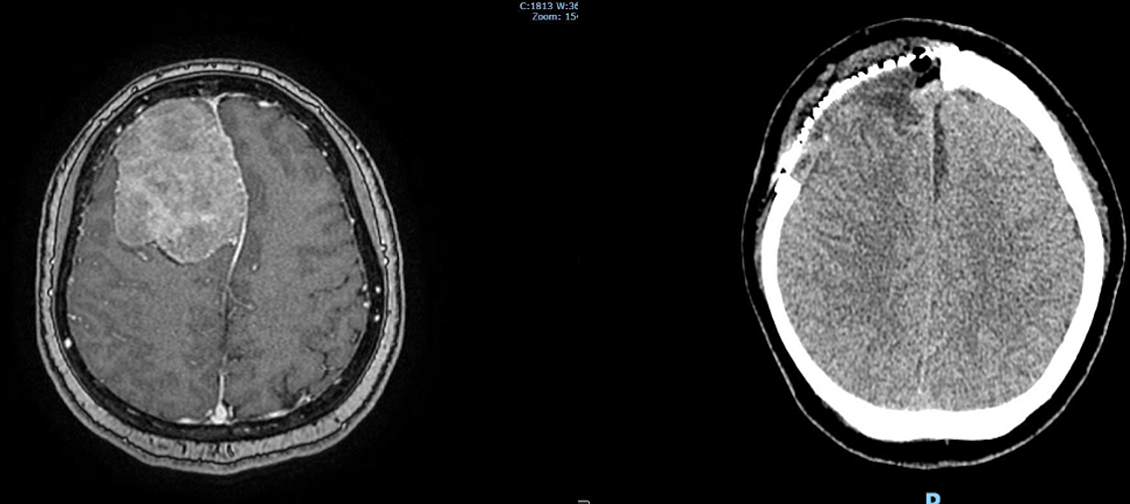 |
Pre-operative MRI showing the orange-sized tumor occupying 25% of the brain (left) and post-operative MRI showing the successful removal of the tumor (right). Photo: Hospital provided |
Pre-operative MRI showing the orange-sized tumor occupying 25% of the brain (left) and post-operative MRI showing the successful removal of the tumor (right). Photo: Hospital provided
Four days post-surgery, the patient's health had recovered to approximately 90%, and her spirits were high. "Initially, my family was shocked, but we realized how fortunate we were that the tumor was detected and treated promptly. I've recovered very quickly," the patient shared.
Doctor Anh explained that the medical team had planned to consult with an oncologist for follow-up care or chemotherapy/radiation if the biopsy revealed malignancy. Fortunately, the tumor was benign, and because the surgeons preserved nearly all of the patient's brain tissue during the operation, she is expected to return to her normal life soon.
Le Phuong












