A recent federal investigation has unveiled disturbing practices in Kentucky's organ donation system, raising serious ethical questions about the Network for Hope, formerly known as the Kentucky Organ Donor Affiliates (KODA). The investigation revealed numerous instances where the organization, responsible for coordinating organ donations in the state, allegedly pressured doctors to prematurely end life support, even when patients showed signs of awareness.
The Network for Hope, a non-profit organization established in 1987, acts as the intermediary between hospitals and the national organ recipient network. Its staff are stationed in hospitals to assess patient conditions, encourage organ donation, and coordinate the entire retrieval process.
While most organ donors in the US are brain-dead, donation after circulatory death (DCD), where patients have some brain activity but are deemed beyond recovery and on life support, is becoming increasingly common. In these cases, if the family consents, life support is withdrawn, and organs are harvested only if death occurs within one to two hours. Doctors must then wait an additional 5 minutes to confirm death.
The Health Resources and Services Administration (HRSA) investigation examined 350 canceled organ donations in Kentucky over 4 years. They found that in 73 cases, organ retrieval plans should have been halted sooner due to signs of patient recovery or awareness. Although organs were not ultimately retrieved, many patients displayed signs of distress during the surgical preparation. Most died hours or days later, but some even recovered and were discharged.
The HRSA discovered that Network for Hope staff frequently pressured families to expedite the donation process, overriding treating physicians and urging hospital staff to remove life support even when patients showed clear signs of awareness. Some staff also misjudged patient conditions due to the effects of sedatives or narcotics, mistakenly believing them to be irreversible.
One case involved Anthony Thomas Hoover II, a Kentucky man who overdosed in 2021. According to a New York Times investigation, although his family agreed to organ donation after two days of unconsciousness, records showed his neurological condition had improved. After struggling in bed during an examination, he was sedated. Concerned hospital staff expressed that the actions resembled "performing euthanasia," but an organ donation coordinator reassured them otherwise. Hoover cried, kicked his legs, and shook his head while being taken for organ retrieval. Ultimately, a doctor refused to withdraw life support, and Hoover survived, albeit with permanent neurological damage.
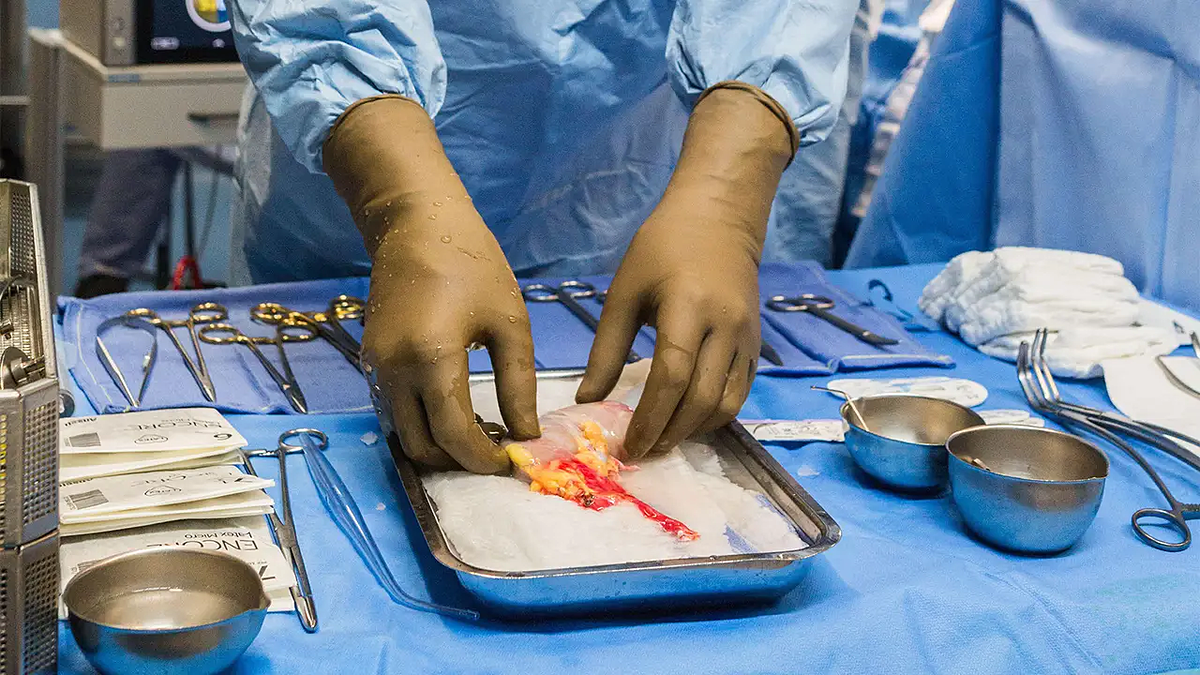 |
Organs during a transplant surgery. Photo: Med Page Today |
Organs during a transplant surgery. Photo: Med Page Today
In another incident in 12/2022, a 50-year-old man who suffered a drug overdose began moving and looking around less than an hour after life support was withdrawn. The surgical team didn't stop immediately, and the patient received no explanation. The transplant was canceled only when his organs became unsuitable. He died three days later after speaking with his family.
Former employees confirmed that superiors had pressured doctors to continue the organ retrieval process. "If it wasn’t for that doctor, we would have 1,000% proceeded," stated Natasha Miller, a staff member present in the room. Three others reported witnessing similar situations.
The investigation also documented cases where staff expressed "extreme discomfort" with patients' neurological responses. In several instances, despite patients' clear reflexes causing distress among medical personnel, preparations for organ retrieval continued.
The investigation highlighted 103 questionable cases, noting that errors were more frequent in rural hospitals. Over 50% of Network for Hope's transplants came from DCD patients, higher than the national average.
In response, Network for Hope claimed adherence to protocol, stating they only retrieve organs after hospitals declare death. However, they agreed to implement new federal requirements: neurological assessments of potential donors at least every 12 hours, retraining all staff on organ donation procedures, and empowering any individual involved to halt the process upon detecting patient irregularities.
On 22/7, before the US House Energy and Commerce Committee, HRSA leadership called for increased transparency and oversight. Committee Chairman Brett Guthrie stressed, "This is a model that puts patients at risk." The Kentucky organ donation scandal has sparked a national debate about ethics, procedures, and transparency within the US transplant system.
Thuc Linh (People, Guardian, Advisory, AP)












