Tung, 41, and his wife recently welcomed a healthy baby girl, marking the end of an eight-year journey through infertility. The couple achieved parenthood through successful micro-TESE microsurgery and in vitro fertilization (IVF) at IVF Tam Anh, a specialized reproductive assistance center in Hanoi.
Tung's path to fatherhood was particularly challenging. He had previously undergone unsuccessful sperm retrieval surgery, leading doctors to suggest donor sperm for IVF. This difficulty contributed to the end of his first marriage. In 2024, Tung remarried a woman three years his junior, who also had a previous failed marriage and a history of miscarriage.
The couple sought help at the Center for Reproductive Assistance, Tam Anh General Hospital Hanoi (IVF Tam Anh). Associate Professor, Doctor Le Hoang, the Center's Director, diagnosed Tung with azoospermia and noted his very small testicles. Genetic tests revealed no abnormalities. His wife presented with diminished ovarian reserve and a blocked left fallopian tube, adding to the complexity of their case.
Doctor Hoang described the case as difficult, citing the couple's age and long history of infertility. However, Tung still had hope for biological children because his spermatogenesis process had not completely ceased. He was recommended for micro-TESE microsurgery to retrieve sperm for IVF, a procedure with a success rate of 40-60% for such cases.
During the micro-TESE procedure, doctors used a microsurgical microscope magnified 25-30 times to directly observe potential seminiferous tubules within the testicular tissue. This allowed for precise sperm collection while minimizing damage to healthy tissue. Tung's left testicle, small and marked by adhesions and fibrosis from prior interventions, yielded no viable seminiferous tubules. After a two-hour search in the right testicle, doctors located several dilated seminiferous tubules with sperm-producing capability, deep within a corner. Six tissue samples were extracted and immediately transferred to a sterile laboratory.
In the embryology lab, specialists used an inverted microscope magnified over 200 times. They identified one field containing 4-5 immotile sperm and six fields with weakly motile sperm. These samples were then activated in a hypotonic solution, allowing for the selection of viable, healthy sperm suitable for IVF. Ultimately, Tung had enough sperm for intracytoplasmic sperm injection (ICSI) to create embryos, with two vials cryopreserved for a potential future cycle.
Doctors retrieved oocytes from Tung's wife, which were fertilized with his sperm, resulting in four day-3 embryos. One fresh embryo was transferred to the wife's uterus, while the remaining three embryos were cultured to day 5 and cryopreserved. Throughout the pregnancy, doctors at the Center for Obstetrics and Gynecology closely monitored the wife, making timely adjustments to her treatment plan to ensure the fetus's safe development. A healthy baby girl was born, weighing 3 kg.
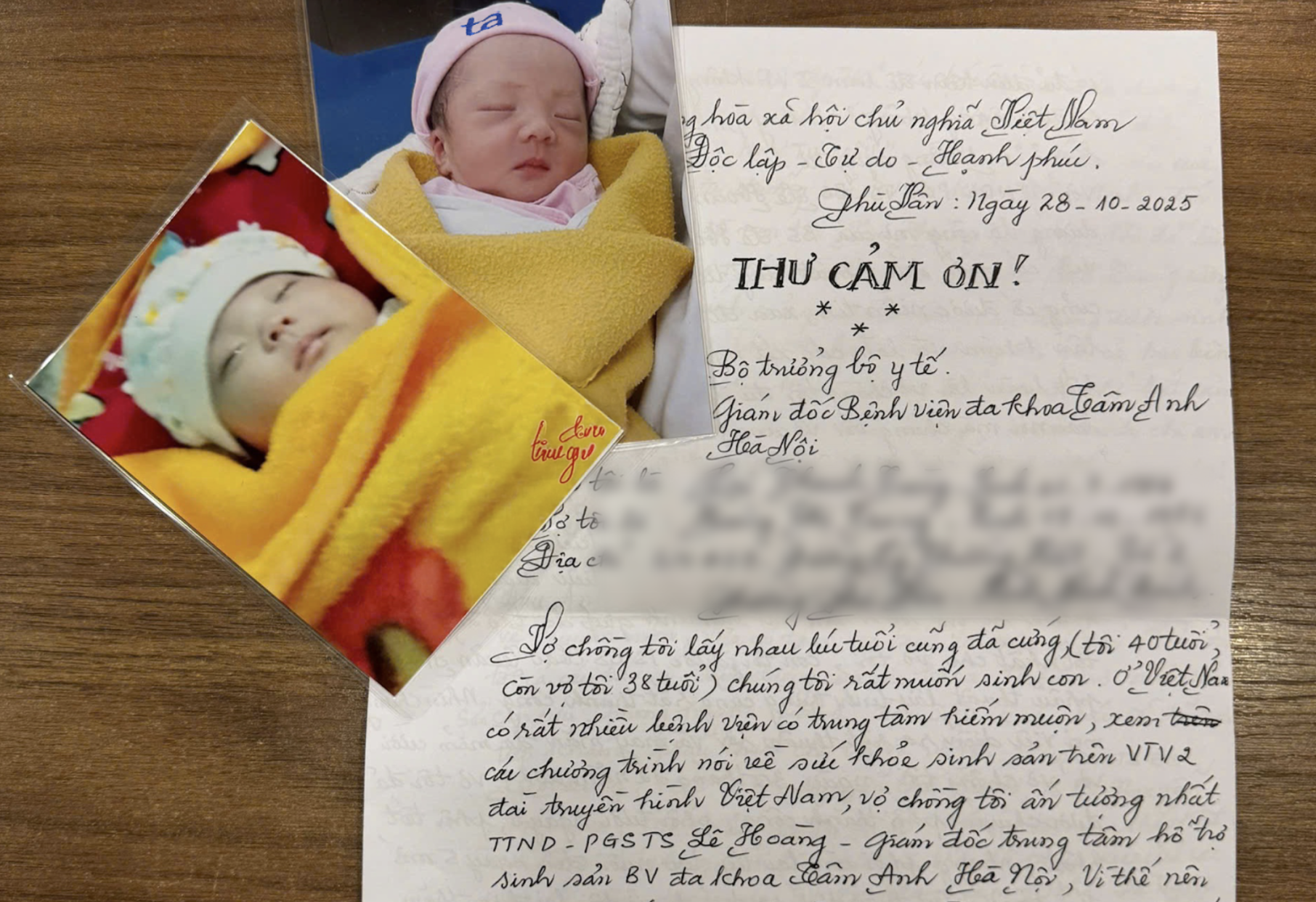 |
A thank-you letter from Tung and his wife to the doctors who helped them have a child. Photo: IVF Tam Anh |
IVF Tam Anh has a track record of successfully treating many azoospermic men, including those with multiple failed sperm retrieval surgeries. Treatment approaches vary based on the patient's condition and the underlying cause. Doctors may recommend micro-TESE microsurgery promptly or opt for medical treatment, followed by a period of testicular tissue recovery before subsequent surgery. Associate Professor Le Hoang noted that this method has helped over 60% of azoospermic patients find sperm, with embryo creation results comparable to using sperm obtained from ejaculate.
Doctors advise men with a history of mumps, genital trauma, sexually transmitted infections, or any reproductive organ abnormalities to seek early examination for timely detection and treatment. Unmarried individuals who discover such abnormalities should consider sperm cryopreservation to preserve their future fatherhood potential.
Trinh Mai