HSV-1, which causes cold sores, affects nearly two-thirds of the world's population. Results from a phase 1-2 trial, published in the *Journal of Clinical Oncology* and presented at the 2025 annual meeting of the American Society of Clinical Oncology, suggest that a genetically modified form of this virus may shrink or eliminate tumors in patients with metastatic melanoma.
The IGNYTE trial, involving 140 patients at Keck Medicine and other global sites, focused on individuals who had not responded or stopped responding to standard immunotherapy. Patients were treated with RP1 (the modified HSV-1) in combination with nivolumab, a standard immunotherapy drug.
The results showed that tumors shrunk by at least 30% in one-third of patients, with approximately 1/6 experiencing complete tumor disappearance. “These findings are encouraging, as melanoma is the 5th most common cancer in adults, and about 50% of advanced cases don't respond to current treatments," said Dr. Gino Kim In, oncologist at Keck Medicine and lead investigator at the trial site.
RP1 is an oncolytic virus, a new class of immunotherapy drugs that can target and destroy cancer cells while activating a systemic immune response. RP1 does not cause herpes. When injected into tumors, it replicates within the cancer cells, destroying them and prompting white blood cells to attack other cancer cells throughout the body.
Along with RP1, patients received nivolumab, which enhances the body's immune response against cancer cells and is expected to make RP1 more effective.
Patients in the study had two or more tumors, including both superficial tumors (on or near the skin) and deep tumors (in the liver or lungs). RP1 was injected into both tumor types. Patients received the combined RP1 and nivolumab treatment every two weeks for up to eight cycles. If they responded to treatment, they continued with nivolumab alone every four weeks for up to two years.
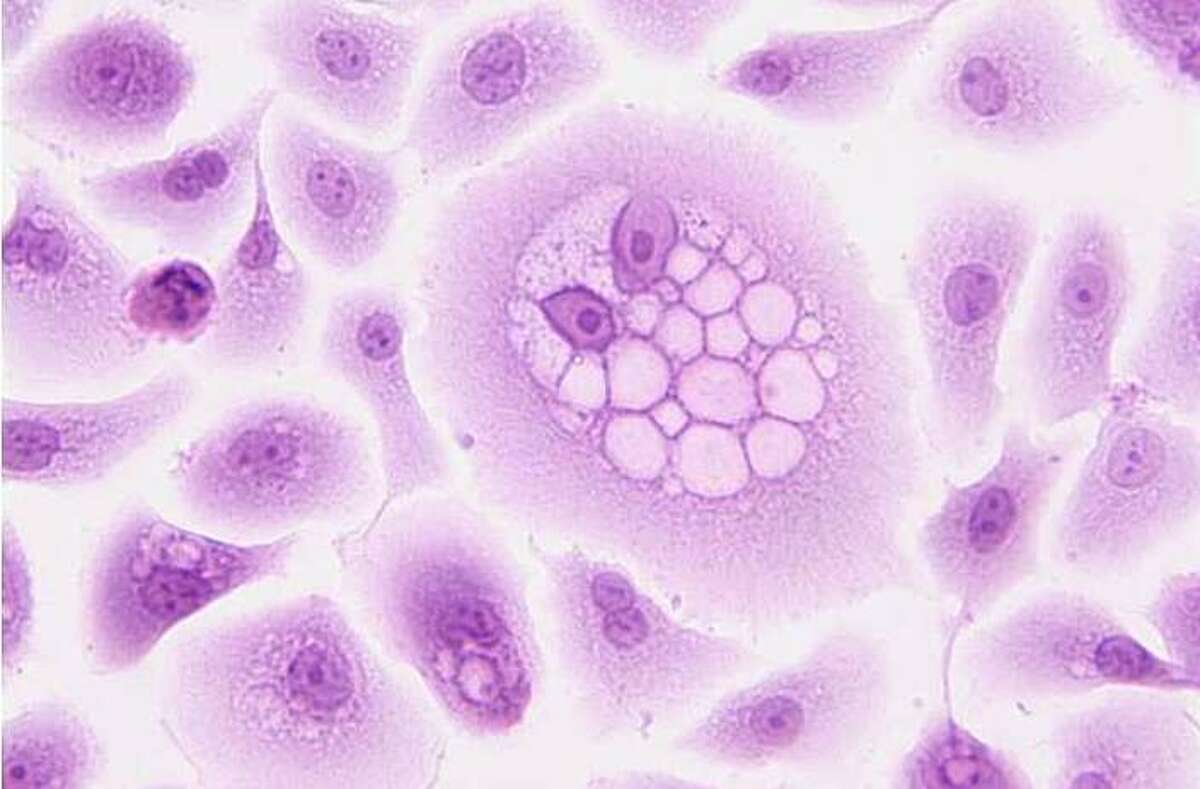 |
Herpes Virus. *Image: MedicalXpress* |
Remarkably, not only did the tumors injected with RP1 shrink, but uninjected tumors also reduced in size or disappeared with similar effectiveness. “This demonstrates that RP1 has a systemic effect, not just a local one at the injection site," said Dr. In.
RP1 was also well-tolerated, with a favorable safety profile. While further evaluation of long-term efficacy is needed, researchers believe this approach could offer a new treatment option for patients who have exhausted other options.
The US Food and Drug Administration (FDA) granted priority review for RP1 in combination with nivolumab in 3/2025. A phase 3 clinical trial, IGNYTE-3, is now underway to confirm the previous results in over 400 patients globally.
In addition to Dr. In, the research team includes Drs. Phillip M. Cheng and Ali Rastegarpour of Keck Medicine. The study highlights the potential of oncolytic viruses in the fight against difficult-to-treat cancers.
Thuc Linh (*MedicalXpress*)












