Radiotherapy is a primary treatment method for lung cancer, alongside surgery, chemotherapy, and more recently, immunotherapy and targeted therapy.
Doctor Bui Le Phuoc Thu Thao, Deputy Head of Radiotherapy Department at the Oncology Center, Tam Anh General Hospital, TP HCM, states that accurate and optimal radiotherapy indications require doctors to determine the disease stage, cancer type, and tumor location. They also assess the patient's respiratory function and overall health. Timely radiotherapy effectively controls the disease, potentially eradicating cancer or providing palliative care. It contributes to maintaining quality of life and extending patient survival.
Lung cancer is categorized into two main types: non-small cell lung cancer (NSCLC), which accounts for about 87% of all lung cancer cases, and small cell lung cancer (SCLC), making up the remaining 13%. Radiotherapy indications differ for these two groups.
For non-small cell lung cancer, radiotherapy is indicated in patients diagnosed early but unable to undergo surgery. This can be due to challenging tumor locations, such as proximity to large blood vessels, mediastinal invasion, or closeness to the trachea. It also applies to patients with severe co-existing conditions.
In early stages, doctors often use stereotactic body radiation therapy (SBRT) as an alternative to surgery. This method controls tumor growth, reduces size, and minimizes side effects. SBRT delivers high radiation doses precisely to the tumor in a limited number of sessions, typically one to five, while sparing healthy lung tissue. This technique is suitable for early-stage primary lung tumors that are small and have not metastasized to lymph nodes.
In advanced tumor stages (stage three), radiotherapy is often combined with concurrent chemotherapy alongside surgery. This is especially true in cases of extensive lymph node metastasis, poor patient health, or when surgery is not feasible. Concurrent chemoradiotherapy is part of a multi-modal treatment approach designed to enhance tumor eradication, limit tumor invasion and metastasis, and extend patient survival.
Post-operative radiotherapy is indicated in certain cases following lung tumor surgery. These include situations where surgical margins contain cancer cells, there is a high risk of recurrence, or extensive lymph node metastasis.
 |
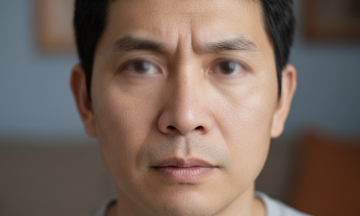
Doctor Thao and a technician encourage a patient before a CT simulation for radiotherapy. *Illustration: Tam Anh General Hospital* |
Doctor Thao explains that with small cell lung cancer, tumors progress rapidly, spread early, and have a high tendency to metastasize to the brain. Consequently, the role of radiotherapy varies across different treatment stages.
In the extensive stage of lung cancer, initial radiotherapy is not typically favorable. If patients respond well to chemotherapy, targeted therapy, or immunotherapy, and the tumor shrinks, doctors may then indicate radiotherapy. This helps reduce recurrence risk and increase survival.
Additionally, in the extensive tumor stage, doctors may prescribe prophylactic cranial irradiation (PCI). This involves low-dose radiotherapy to the entire brain before metastasis occurs, reducing the risk of seizures, hemiplegia, memory impairment, and coma.
In advanced or metastatic stages, the goal of radiotherapy is not curative but primarily palliative. It aims to alleviate symptoms such as pain, hemoptysis, bronchial obstruction, and dyspnea. It also works to prevent spinal cord compression, thus preserving mobility. In some cases of brain metastasis, radiotherapy helps control metastatic lesions, reducing symptoms and improving patient quality of life.
Nhat Minh
| Readers can submit questions about cancer here for a doctor's response. |