Mrs. Tinh, 80, developed a tumor six months ago. It progressively grew, causing her left face to swell, pushing out her cheek and lip, making them uneven and distorted. Inside her mouth, there were sores and discharge. The rapidly growing tumor caused pain, making it difficult for her to speak clearly and eat, leading to a 5 kg weight loss. A biopsy at Tam Anh General Hospital in TP HCM confirmed a 7 cm long, 4 cm thick stage three cheek lining cancer.
"Mrs. Tinh has chewed betel for many years, which could be a risk factor for oral cancer," said Doctor Nguyen Huy Loc, a specialist in radiation oncology at the Oncology Center. This type of cancer often affects older individuals and tends to progress rapidly.
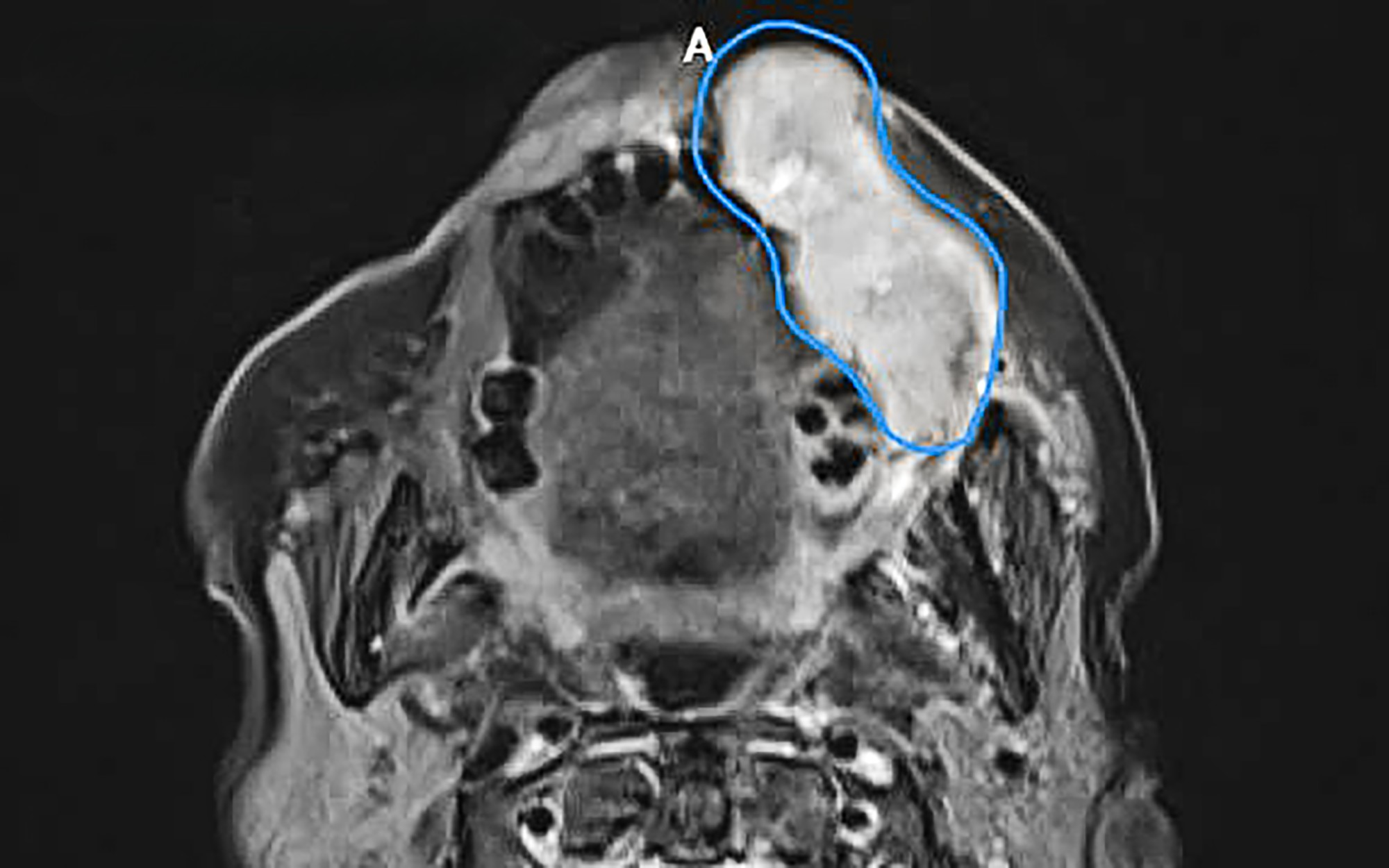 |
CT scan showing a malignant tumor (blue area) invading the cheek and lip from the oral mucosa. Photo: Tam Anh General Hospital
Doctors initially recommended surgical removal of the entire tumor, with wide margins and neck lymph node dissection to ensure all cancer cells were eradicated and to prevent metastasis and recurrence. To avoid a sunken cheek area post-surgery, which would impact chewing, speech, and aesthetics, reconstructive surgery using an autologous skin flap was planned. However, due to the patient's advanced age and multiple underlying health conditions, her family opted for radiation therapy instead of surgery.
Radiation therapy is a non-invasive method that doesn't require continuous hospitalization during treatment, thus avoiding potential surgical complications like those associated with general anesthesia, and often leads to better recovery. Doctor Loc developed a radiation therapy protocol for Mrs. Tinh, consisting of 33 sessions, focusing on the cheek lining tumor and bilateral neck lymph nodes to prevent cancer metastasis and recurrence.
 |
A nurse from the Radiation Oncology Department advises Mrs. Tinh on her next radiation therapy schedule. Photo: Tam Anh General Hospital
The tumor was close to the skin and protruded, causing facial deformity. Therefore, in addition to creating a specialized immobilization mask that conformed to the tumor's shape, doctors designed a bolus (dose compensation plate) to achieve optimal radiation delivery. Strong radiation is most effective when delivered 2-3 cm below the skin surface. In this patient's case, as the tumor had spread to the lip area, a 1 cm thick hard plastic bolus was used. This bolus acted as a tissue layer covering the tumor, helping the radiation beams hit the target precisely and minimizing damage to healthy tissue beneath the tumor.
After five radiation sessions, the patient responded well: the tumor significantly reduced in size, pain decreased, and she could chew and speak more easily. The protruding tumor in her mouth disappeared, and her facial appearance was nearly normal. Before subsequent radiation sessions, the patient's immobilization mask and bolus were refitted to ensure a snug fit with the treated area.
Oral cancer is commonly observed in individuals over 50 who regularly smoke, consume alcohol, chew betel nut, maintain poor oral hygiene, or suffer from chronic, untreated ulcers. The disease is often detected in late stages (3 or 4) because initial symptoms are vague and easily mistaken for common canker sores or infections.
Doctor Loc emphasized that treating late-stage cancer carries a worse prognosis compared to early stages, affecting both treatment success and quality of life. Patients should seek immediate medical attention if they notice any unusual signs, such as swelling or pain in the mouth area. Regular dental check-ups, once every 6-12 months, are essential for timely detection and treatment of any abnormalities.
Nhat Minh
*Patient's name has been changed.
| Readers can submit their cancer-related questions here for doctors to answer. |












